Pericardial Injection Effective, Less Invasive Way to Get Regenerative Therapies to Heart

Injecting hydrogels containing stem cell or exosome therapeutics directly into the pericardial cavity could be a less invasive, less costly, and more effective means of treating cardiac injury, according to new research from the NC State University and the University of North Carolina at Chapel Hill.
Stem cell therapy holds promise as a way to treat cardiac injury, but delivering the therapy directly to the site of the injury and keeping it in place long enough to be effective are ongoing challenges. Even cardiac patches, which can be positioned directly over the site of the injury, have drawbacks in that they require invasive surgical methods for placement.
“We wanted a less invasive way to get therapeutics to the injury site,” says Ke Cheng, Randall B. Terry, Jr. Distinguished Professor in Regenerative Medicine at NC State College of Veterinary Medicine’s Department of Molecular Biomedical Sciences and professor in the NC State/UNC-Chapel Hill Joint Department of Biomedical Engineering. “Using the pericardial cavity as a natural “mold” could allow us to create cardiac patches – at the site of injury – from hydrogels containing therapeutics.”
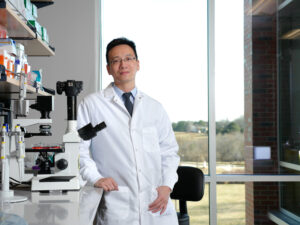
In a proof-of-concept study, Cheng and colleagues from NC State and UNC-Chapel Hill looked at two different types of hydrogels – one naturally derived and one synthetic – and two different stem cell-derived therapeutics in mouse and rat models of heart attack. The therapeutics were delivered via intrapericardial (iPC) injection.
Via fluorescent imaging the researchers were able to see that the hydrogel spread out to form a cardiac patch in the pericardial cavity. They also confirmed that the stem cell or exosome therapeutics can be released into the myocardium, leading to reduced cell death and improved cardiac function compared to animals in the group who received only the hydrogel without therapeutics.
The team then turned to a pig model to test the procedure’s safety and feasibility. They delivered the iPC injections using a minimally invasive procedure that required only two small incisions, then monitored the pigs for adverse effects. They found no breathing complications, pericardial inflammation, or changes in blood chemistry up to three days post-procedure.
“Our hope is that this method of drug delivery to the heart will result in less invasive, less costly procedures with higher therapeutic efficacy,” Cheng says. “Our early results are promising – the method is safe and generates a higher retention rate of therapeutics than those currently in use. Next we will perform additional preclinical studies in large animals to further test the safety and efficacy of this therapy, before we can start a clinical trial.”
“I anticipate in a clinical setting in the future, iPC injection could be performed with pericardial access similar to the LARIAT procedure. In that regard, only one small incision under local anesthesia is needed on the patient’s chest wall,” says Dr. Joe Rossi, associate professor in the division of cardiology at UNC-Chapel Hill and co-author of the paper.
The research appears in Nature Communications and was supported by the National Institutes of Health and the American Heart Association. Dr. Thomas Caranasos, director of adult cardiac surgery at UNC-Chapel Hill, also contributed to the work.
Tracey Peake/NC State News Services