NC State College of Veterinary Medicine Researcher Uncovers Bartonella, the ‘Stealth Pathogen’
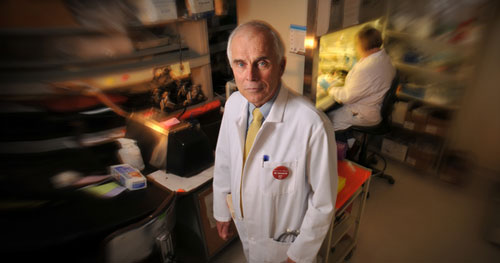
Dr. Ed Breitschwerdt is an expert on infectious diseases and a doctor of veterinary medicine. He also finds himself on the front lines of a quiet but growing epidemic. Bartonella is a bacteria most commonly associated with cat scratch disease, which until recently was thought to be a short-lived (or self-limiting, in medical lingo) infection. Bartonella isn’t new – doctors have known about cat scratch disease for almost a century – but it’s only in the past couple of decades that researchers like Dr. Breitschwerdt have started to discover exactly how pervasive Bartonella infecton is in animals and people.
“The main problem with determining whether Bartonella is involved with a particular illness has traditionally been the difficulty of culturing the bacteria from patient samples,” Dr. Breitschwerdt says. Some of his earliest work was simply dedicated to finding a better way to identify the presence of the bacteria in an animal or human. It’s fairly easy to find evidence of Bartonella in “reservoir hosts,” or the animals that harbor the bacteria: currently, researchers use a combination of serology and PCR (which stands for polymerase chain reaction) to identify Bartonella’s bacterial DNA in samples.
Finding it in potentially infected humans, however, takes a bit more specialized testing. Dr. Breitschwerdt had to develop a specialized growth media in order to be able to culture the bacteria in numbers great enough to detect using a standard PCR test.
Once Dr. Breitschwerdt and other researchers had the proper tools to look for evidence of the bacteria they found that Bartonella is literally all around us.
“We have found species of Bartonella in mammals ranging from mice to sheep to sea otters to dolphins,” he says. “There are at least 30 different species that we know of right now, and 13 of those have been found to infect human beings.”
Of course, the likelihood of a human contracting Bartonella from a sea otter is low. But several Bartonella species have found a home much closer to home – in domestic dogs, cats, cows, and rodents which can act as bacterial reservoirs. Fleas, lice – and possibly ticks – also act as repositories for different strains of the bacteria.
Okay, so these bacteria can be found everywhere. People have been getting cat scratch disease for a long time, and it’s usually not that big a deal. What’s changed?
One answer is that our ability to find and diagnose Bartonella infection in animals and humans has led to its identification in patients with a host of “chronic illnesses” that the medical community previously hadn’t been able to attribute to a specific cause. Whether these bacteria cause these chronic illnesses is yet to be determined.
There is an increasing body of research linking the Bartonella bacteria to a number of chronic ailments ranging from migraines to seizures to rheumatoid illnesses to endocarditis, which is the inflammation of the valves of the heart.
The way Bartonella works in your body goes something like this: Once a human is infected by an animal bite or scratch, or by an arthropod – like a flea or tick – bite, Bartonella takes up residence in red blood cells and endothelial cells – the cells that line blood vessels. This serves as a great hiding place for the bacteria, which can then cause cycles of repeated intravascular infection (known as cyclic bacteremia), ultimately affecting multiple organs and organ systems. The ability of these bacteria to hide within cells makes diagnosis and treatment tricky.
The medical evidence seems to support the anecdotal evidence that first drew Dr. Breitschwerdt’s interest in the topic: veterinarians suffering from chronic illnesses that were often diagnosed as Lyme disease or chronic fatigue, or in one extreme case, multiple sclerosis. A persistent bacterial infection can result in many of these same symptoms.
Okay, so the evidence suggests that this little bug can cause a lot of problems. Who’s most at risk, and what’s the treatment?
Veterinarians and people with high rates of exposure to farm animals, domestic animals and arthropods like fleas and lice are the most at risk, according to Dr. Breitschwerdt. “These individuals should take care to avoid arthropod bites, arthropod feces, animal bites or scratches, and direct contact with bodily fluids from sick animals,” he says. Additionally, Dr. Breitschwerdt has published evidence that Bartonella infection can be transmitted from mothers to infants at birth.
Antimicrobial drugs that can enter the cell are used most frequently for treating Bartonella infection in humans, but the infection has not been eliminated in all patients treated with antibiotics that should be effective. There is increasing evidence of treatment failures in people with normal immune systems, and it is not uncommon to see relapses in immunocompromised patients who were treated for six weeks or longer.
This past April, NC State University hosted the 7th annual international conference on Bartonella as human and animal pathogens. Over the course of the four-day conference, medical professionals and researchers from around the world gave presentations on topics ranging from rates of Bartonella infection in healthy dog and cat populations, to close examinations of the morphology, or structure, of Bartonella inside cells.
A lot of the research presented dealt with the main issue that confronted Ed Breitschwerdt when he first began looking closely at Bartonella – the stealthy nature of the pathogen and its ability to conceal itself within the human body, even while causing repeated illnesses.
Dr. Lesley Ann Fein, a rheumatologist who attended the conference, offered a very nice summary of both the conference and its implications for future research:
“Bartonella bacteria are highly evolved, survive in multiple insect vectors and in dessicated flea feces, and enter our bodies in a stealth-like manner, switching off our immune response as it takes residence in our tissues.
“It persists despite aggressive treatment and is clearly a contender for diseases transmitted by blood transfusions. Physicians must be cognizant of the stealth nature of this pathogen and the alarmingly high frequency of seronegativity.”
Dr. Breitschwerdt agrees. “We need to understand more about the way this bacteria functions in the human body – how and why it is so successful at hiding and causing persistent infections. We also need to get the word out to the medical community about this pathogen. Just knowing what to look for may end up giving patients with unexplained chronic illnesses better treatment options.
“In my opinion, bartonellosis, caused by the diverse members of the genus Bartonella, may prove to be the most important emerging infectious disease of the next decade.”
[section_subtitle] For more information: [/section_subtitle]
NC State CVM Bartonella Research Publications
Intracellular Pathogens Research Lab Advances Understanding of Bartonella
Bartonella Infections May Lead to Possible Birth Defects
Bartonella: Emerging Infectious Disease
Tracking a ‘Stealth’ Pathogen
Bartonella Questions for Dr. Breitschwerdt


