Quantifying Bartonella Risks to Veterinarians
Dec. 1, 2010
By: Daniel R. Verdon, DVM NEWSMAGAZINE
National Report — Bartonellosis: It’s no longer considered a self-limiting disease, and for some people chronic infection can be as debilitating and hard to diagnose as Lyme disease.
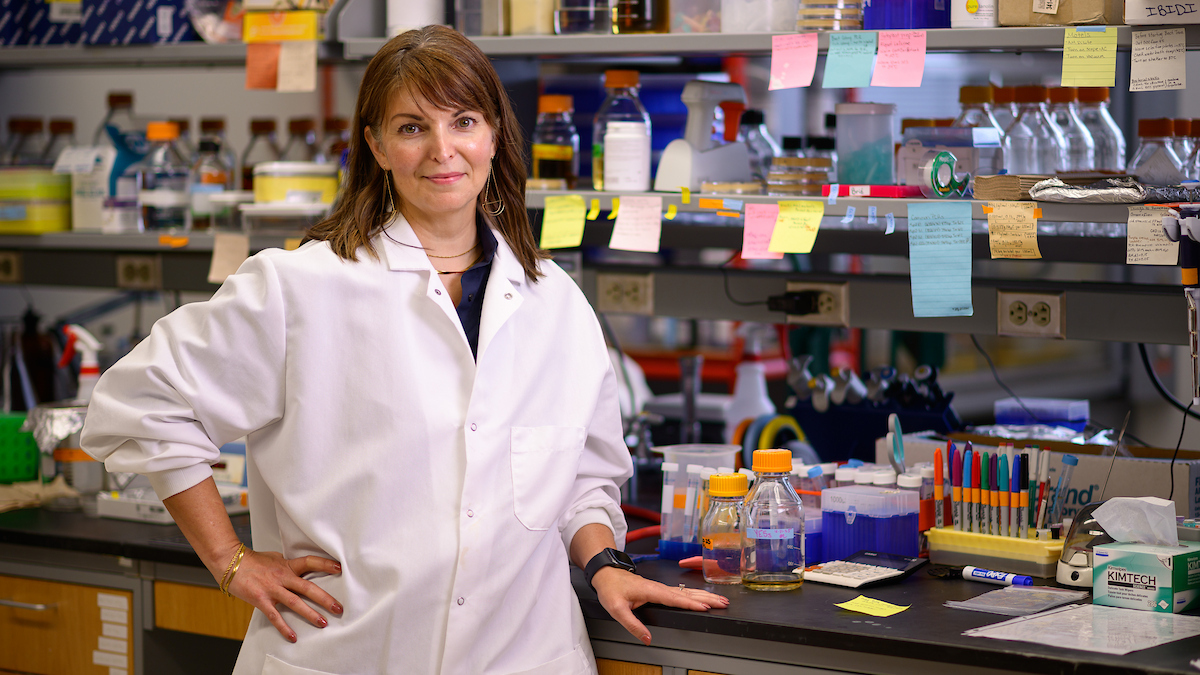
While new human medical and veterinary research is quickly debunking traditional beliefs about these infectious bacteria, expert Dr. Edward Breitschwerdt, of North Carolina State University’s College of Veterinary Medicine, wants veterinarians to sit up and take notice. The health risks appear to be very real, and they are heightened by frequent contact with sick animals.
“Going from not knowing a genus of bacteria existed in the 90s to now realizing that cats, dogs, cows, deer, squirrels, voles, moles and kangaroos in Australia are all running around with their own Bartonella species in their blood changes the dynamics of the human-animal bond. And it creates some caution that we didn’t have to worry about five years or 10 years ago when we didn’t know this information.”
Dr. Breitschwerdt has spent much of his professional career studying vector-borne infectious diseases. And while cat-scratch disease was recognized nearly 100 years ago, the bacteria that causes this and other Bartonella-related disease manifestations and the routes by which humans become infected needs much more research. What is known is that Bartonella henselae, B. clarridgeiae, B. koehlerae can be transmitted by infected fleas and the inoculation of flea feces. The infected nail beds and saliva of cats are routes of transmission following a bite or scratch,” Breitschwerdt says. And persistent intravascular infection in some individuals can result in a cascade of medical conditions like arthritis, endocarditis, encephalitis and others (Tables 1 and 2).
To continue to read the article from DVM NEWSMAGAZINE and view Tables 1 and 2, click here.