One of the Family: Animal Care Drives CVM Innovations
How devotion to our pets is changing veterinary medicine… and improving human lives
The following article is reprinted from the Winter 2009 issue of the NC State Alumni Magazine. Join the Alumni Association to obtain the magazine and other membership benefits.
In a small hospital room in Raleigh, Serena Van Dyke lies on her side on a metal table. She’s covered with a white blanket. Two IV lines circle from her neck to a beige machine with spinning black knobs.
Serena has lymphoma. She’s only 5 years old. With chemotherapy alone, she wouldn’t live past 7. The machine is siphoning a type of white-blood-cell population rich in stem cells, which can become any sort of cell. Her oncologist will use those stem cells to repopulate her bone marrow and, he hopes, cure her cancer.
A shepherd from Houston, Texas, Serena is here because Dr. Steven Suter was sick of watching dogs die. Theyd come to NC State’s Veterinary Teaching Hospital to be treated for lymphoma, but Suter, an assistant professor of oncology, could only offer to buy a little time with chemotherapy. Lucky patients would have a decent quality of life for a year or so. Then, a recurrence. The cure rate with chemo for dogs is only 2 percent, or, as Suter says, “almost nothing.” He remembers a pet owner, one of the many who had spent nearly $10,000 on chemo for a dog who would almost certainly die, asking him: Is that all you have? “That guy stuck with me,” Suter says.
When chemo fails humans with lymphoma, a bone marrow transplant increases the cure rate to up to 60 percent. It’s a procedure that scientists had actually perfected in dogs before it made its way to human hospitals. So Suter, who owns a pit bull named Curbside and a boxer named Alamo, set out to start the country’s only clinical canine bone marrow transplant program.
“It wasn’t a stretch for me to wonder if people would be willing to spend an extra $5,000 or $6,000 with a chance of being able to completely cure [their dog’s disease],” Suter says. He was right. Serena is the 13th dog to receive a bone marrow transplant at NC State in less than a year. The program has a waiting list; Serena was on it for 5 months. “She is only 5 years old, and I love her very much,” says Serena’s owner, Scott Van Dyke. “German shepherds have a normal life span of 10 to 13 years. I knew if we did this and it was successful, it would give her another five to seven years.”
That demand is just one product of the way human devotion to pets is changing veterinary medicine. Animals were domesticated as workers, but as we’ve shifted from an agrarian to an urban society, they’ve become something else. More and more, people treat their pets as if they were their kids. In 2006, nearly half of pet owners considered their pets family members, according to a survey from the American Veterinary Medical Association (AVMA). About half said their animals are companions. Only 2 percent considered them property.
For most, that affection hasn’t translated into big expenses. American households on average spent only $366 for veterinary care for all their pets in 2006, according to the AVMA.
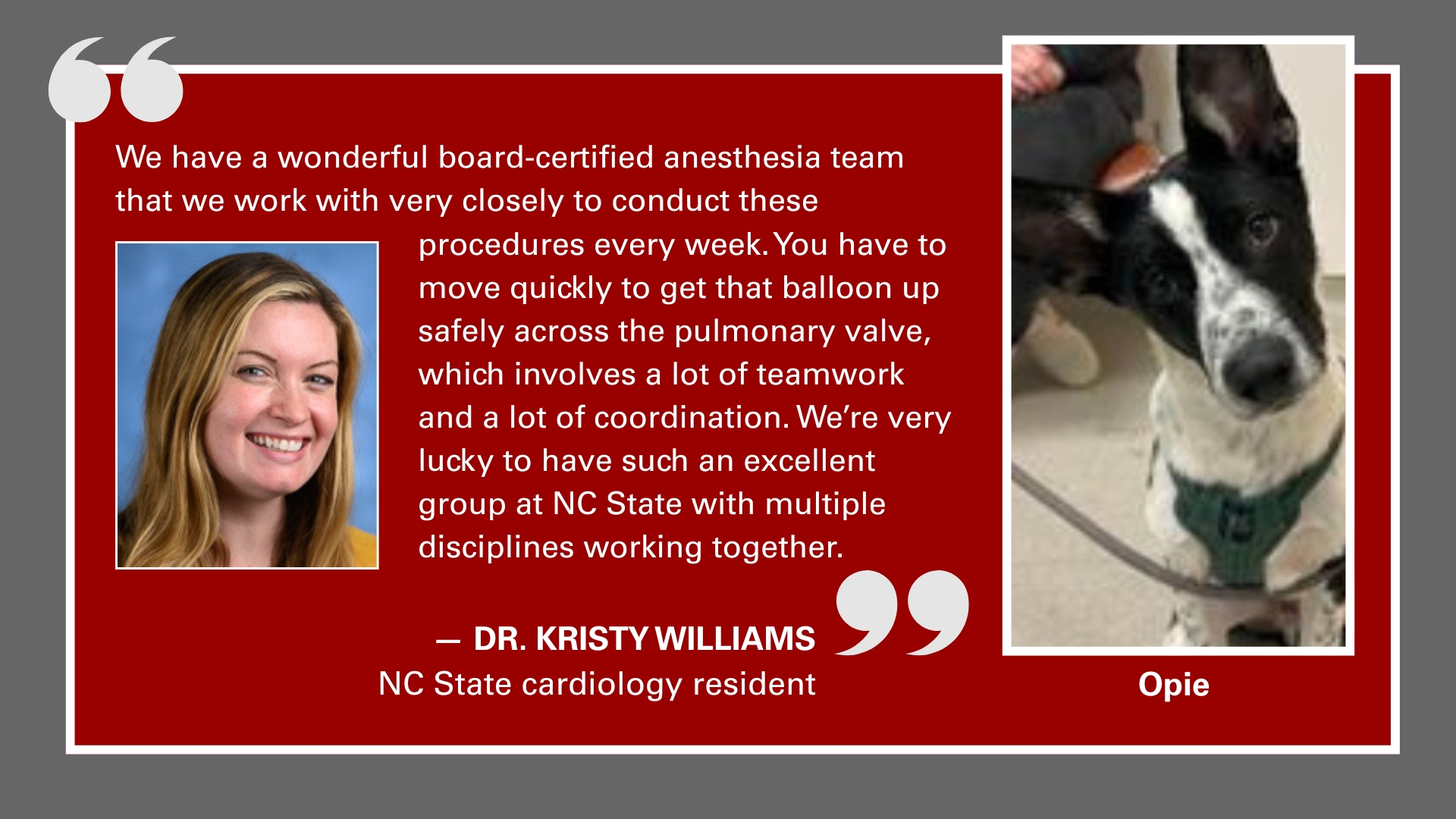
But a minority of pet owners wants the best of everything for their pets, including medical care. Increasingly they can get it. At NC State’s Veterinary Teaching Hospital, the list of services available includes MRIs, CT scans, chemotherapy, radiation, cataract surgery, cardiac catheterizations, knee and hip replacements, and consultations with behaviorists and nutritionists.
Patients come to NC State only on referral from a general-practice vet, so they’re here because their owners are willing to treat them for serious diseases. That’s consistent with a Michigan State University study showing that a steady increase in inflation-adjusted spending on veterinary care between 1980 and 2005 could be attributed to the same households that had already been spending money on vet care. They were just spending more. “Veterinary medicine is a business, and it has responded to a demand,” says Dr. Michael Davidson, a veterinary ophthalmologist and associate dean of veterinary medical services at NC State.
What’s behind that demand? Increases in population and income certainly play a role. Some veterinary researchers attribute it to a societal shift, contending that pets became more important as Americans began having smaller families, getting divorced more often—or not marrying at all—and living longer and having more empty-nest years. Advances in technology also contribute. As specialty treatments like bone marrow transplants mature, they can be made more affordable for pet owners, who spend out of pocket, rather than rely on insurance, as human patients do.
The many different ways that people relate to their animals mean that veterinarians have to think about much more than making sure pets are up to date on vaccines. “Veterinarians will meet owners who see their animals as their sole contact in their life, a family member,” says Dr. Diane Dunning, director of the college’s Animal Welfare, Ethics and Public Policy Program. “Then we’ll get the other end of the spectrum where people don’t like an animal’s color or don’t think it’s behaving appropriately and will abandon the animal or relinquish it to the shelter.” At NC State’s vet school and many others, students are required to take a class on the human-animal bond, where they learn about a variety of ethical issues and discuss how even their own opinions differ depending on culture, geography and experience.
But growth at the hospital is driven almost entirely by people who fall into the pets-as-family category. When the hospital opened in 1983, doctors saw 4,000 cases. By 2008, the caseload had reached 20,000, far outpacing the 46,000-square-foot building’s intended capacity of 13,000 cases.
That will change in late 2010 with the completion of the Randall B. Terry Jr. Companion Animal Veterinary Medical Center, which will add 110,000 square feet to the hospital, with separate areas for its 16 specialties. The Terry Center itself will be a symbol of one pet owner’s devotion. Terry, the former publisher of The High Point Enterprise, was a hospital client who considered his seven golden retrievers his closest family. When he died in 2004, his estate pledged $20 million for the center. (The rest of the $72 million cost will come from other private funds and from $38 million appropriated by the state.)
Until the new facility opens, some corridors of the current hospital are filled with cubicles for residents and technicians, and a couple of bathrooms have been converted to offices and storage closets. A number of services use leased off-campus space. Oncology is a particularly busy specialty, with 4,000 visits in 2008, including repeat patients. Neurology logged 2,800 visits, and cardiology 1,500.
The growing appetite for specialty care is evident in the hospital’s ophthalmology service. When Davidson came to the vet hospital in 1984 for an internship and an ophthalmology residency, the specialty was just starting at NC State and consisted of two faculty members and one resident. They shared one technician with the other services. Now, ophthalmology has three technicians all its own, four faculty ophthalmologists and three residents. Like many of the hospital’s specialists, the ophthalmologists mostly treat dogs (70 percent of the hospital’s patients are canines), followed by cats and horses. But they’ve also removed cataracts and treated glaucoma in fish, chimpanzees, ostriches and even a monitor lizard.
In some cases, experimental treatments available to these pet owners who want to exhaust every available resource are even more advanced than humans can get. Case in point: Dr. Denis Marcellin-Little, associate professor of orthopedics in the College of Veterinary Medicine, works with biomedical engineering associate professor Ola Harrysson to craft custom prosthetic-limb implants that permanently fuse to the bone (called osseointegrated implants). In 2005, Marcellin-Little implanted two cats—George Bailey and Mr. Fonz—with prostheses. In 2009, he installed one for Cassidy Posovsky, a shepherd mix who was the first dog in the world to receive such an implant.
The process of crafting custom implants is partly subsidized by research grants, but it can cost the client $6,000 to $10,000. Steve Posovsky, a retired dentist, says his dog was worth it. He adopted Cassidy after seeing him on the news, emaciated, with a skimpy coat and only three legs. A few months later, he found Marcellin-Little through an Internet search and drove Cassidy from New York to be fitted with a regular, slip-on prosthesis. They tried two different versions; the second one included a custom liner and took a year to make. But Cassidy kicked them both off before leaving the hospital. “It’s like having no foot, then putting a sock on the leg and trying to put on a running shoe,” Marcellin-Little says. The permanent prostheses, which require two operations, became the next step. As Posovsky talks about it by phone, Cassidy and Bella, his Rhodesian Ridgeback, sit beside him in bed. “Anybody would say I’ve gone way over the top for this dog,” Posovsky says. “But the joy of watching him play on the beach like a normal dog and not plop down after five or 10 minutes to have to take a rest—I can’t explain it. It gives me pleasure that only my children could equal.”
Marcellin-Little is confident his work with Cassidy and other pets will someday be applied to people and enable the replacement of any bone that needs it. In the lab, Marcellin-Little, Harrysson and biomedical engineering researcher Elizabeth Loboa have investigated how human stem cells react to the different textures of titanium used for the implants, which will tell them a lot about how human skin and muscle tissue will accept the implants. They presented that research to the Orthopaedic Research Society. In September 2009, the team gave a talk on the prosthetics work to doctors, residents and medical students at Duke University Medical School. “At some point the work in animals and in humans becomes one and the same,” Marcellin-Little says.
Dogs and humans, are, in fact, a lot alike at a genomic level. As the line between human and animal family members may be blurring, so is the line between what constitutes research to benefit pets and research to benefit people. For example, in 2009, genomics professor Matthew Breen narrowed the search for a culprit in one type of human brain cancer by comparing canine and human genomes. Because dog DNA is similar to ours, he could pinpoint smaller regions of genes shared in both species to look for clues, rather than randomly looking at an entire human chromosome. Using this approach, Breen found that a gene commonly believed to be involved in meningiomas, which account for one out of four adult brain tumors, may not be as important as once thought.
Discoveries like Breen’s are making the veterinary hospital more like a research hospital for humans. While exploring better ways to prevent and treat inflammatory bowel disease (IBD) in pigs—a problem that can stunt their growth and even kill them—Adam Moeser, an assistant professor of pig health and production, is learning about the sources of IBD and other stress-related diseases in humans. Pigs make better models for human digestive diseases than mice do, Moeser says. That’s because pigs, like humans, are born with well-developed immune and digestive systems. In mice, much of that development happens after birth. Moeser found that when a pig gets stressed, cells linked to allergic responses, called mast cells, release their contents into the intestinal lining. Now he’s identifying the specific chemicals the mast cells release that may contribute to IBD. “With that knowledge, we can identify certain factors that are important to causing gut dysfunction, then potentially we can inhibit those factors,” he says.
Another example: Attempts to develop a vaccine for human immunodeficiency virus (HIV) have been underwhelming. But the U.S. Department of Agriculture in 2002 approved the vaccine against the feline immunodeficiency virus (FIV), though its efficacy is still being determined. Veterinarian and immunopathologist Gregg Dean collaborates with Todd Klaenhammer, professor of food science, microbiology and genetics, to use lactobacillus (a bacterium that lives in the digestive tract) as a delivery agent for the FIV vaccine. If successful, the method could be used for other types of vaccines, and not just in cats. “We know lactobacillus interacts with the immune system, and it’s safe,” Dean says.
He and Klaenhammer think they can use it to enhance the immune systems response to FIV or HIV. Making such translations between human and animal medicine intentional is the goal of the Center for Comparative Medicine and Translational Research, which Dean directs. The center, which has more than 100 members, connects researchers from many different disciplines so they can more quickly translate ideas from the lab to the patient. It provides access to technology, collects and stores patient samples, and runs clinical trials.
Suter, a member of the translational research center, partners with a UNC-Chapel Hill geneticist to study cells from some of his lymphoma patients to find similarities between dog and human lymphoma. But while owners of the dogs in the bone marrow transplant program are happy if they can help advance cancer research, what they really want are a few more good years with their beloved pets. How many of them will get it? Suter is confident he’ll give some the chance; when dogs were the test subjects in developing human bone marrow transplants, their cure rate was 30 percent. Suter has performed dog transplants since October 2008. Once a patient stays in remission for two years, he can declare the dog officially cured.
But there are no guarantees. As Suter tends to Serena Van Dyke, he wears a white coat embroidered “The Maverick Altman Coat of Excellence.” Maverick, a Weimaraner from Connecticut who had leukemia, was the third dog to get a bone marrow transplant at NC State. He died from complications of his disease in April 2009. (The coat recognizes the $10,000 donation Maverick’s owners made to the bone marrow transplant program.)
As for Serena, the day after her stem-cell harvest, she had two sessions of full-body radiation, which killed any lurking cancer but also destroyed the white blood cells in her bone marrow. Then she got her own stem cells back, via another IV. She recovered in the hospital for three weeks, then her owner, Scott Van Dyke, drove her the 19 hours back to Texas. After six weeks at home, Serena is back to her old self, Van Dyke says, barking at strangers and chasing his three other shepherds around the yard.
She has had one setback: About two weeks after she left the hospital, she crashed. “She had stopped drinking; she wouldn’t move. I didn’t know if she was going to live,” Van Dyke says. She recovered after getting IV fluids in an emergency clinic over a weekend. Now Van Dyke limits her yard time so she won’t overdo it.
He’s confident she’ll be fully cured; he’s already called the Ronald McDonald House to arrange for Serena to work there as a therapy dog. “I’m just waiting for her to get a little bit stronger,” he says. “Then she can become a service dog, to encourage children and adults who are looking at having transplants themselves.”
Angela Spivey is a freelance writer who lives in Fayetteville with her three dogs and four cats.