New NC State Research Partnership Fighting Biofilm-Associated Infections
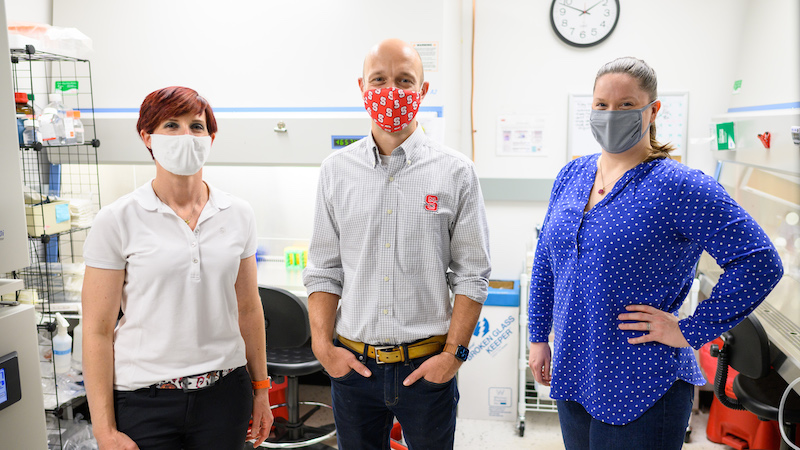
Lauren Schnabel and Joshua Pierce had never worked together before, but their first collaboration may be a giant leap forward in treating common but often life-threatening infections in animals and humans.
Schnabel has joined forces with Pierce to develop and test new classes of antibiotics with the ability to fight drug-resistant infections complicated by bacterial biofilms.
Schnabel is an associate professor of equine orthopedic surgery at the NC State College of Veterinary Medicine, and Pierce is an associate professor of chemistry in the NC State College of Sciences.
The project, with an end goal of commercializing antimicrobial drugs, recently received a pair of two-year grants totaling $1.2 million from the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health.
“This collaboration is crucial and critical to creating new treatments,” says Pierce. “It is an essential union to advance the molecular compounds. Ultimately, it’s the models Lauren and her team will study that will allow us to have the data to say we know these compounds work.”
Through his start-up company Synoxa Sciences, founded at NC State, Pierce and his research team are in the early stages of creating molecular compounds for the project that work against biofilms. Very few small molecules with the ability to directly fight biofilm-associated infections have previously been isolated, says Pierce.
Schnabel and her team will then study the compounds in animal models to evaluate their effectiveness in targeting biofilm-implicated orthopedic infections.
Biofilms are bacterial communities encapsulated in a matrix that makes it difficult for antimicrobials to kill the bacteria. An estimated 80% of medical infections in humans involve biofilm-associated microorganisms. As in humans, biofilms in animals can complicate the effectiveness of implants or prosthetics, possibly leading to more surgeries, amputations and even death.
Schnabel and Pierce’s collaboration would likely have never happened without NC State’s Comparative Medicine Institute. The CMI fosters interdisciplinary research teams whose projects show promise in converting scientific discoveries into clinical applications with translational potential, benefitting both animal and human health.

Pierce, who co-directs the CMI with Jorge Piedrahita, the Randall B. Terry, Jr. Distinguished Professor of Translational Medicine, first learned of Schnabel’s research during a meet-and-greet at the CMI. Jessica Gilbertie, now a postdoctoral fellow in Schnabel’s lab, discussed the group’s ongoing orthopedic injury and biofilm research.
That work at the CVM resonated with Pierce. While Pierce’s work is geared toward treating all types of biofilm-implicated infections in humans, Schnabel and Gilbertie’s focus on orthopedic injury helped tailor the new grant-funded project.
“That’s the beauty of the CMI,” says Schnabel, who co-directs the CMI’s functional tissue engineering program with NC State biomedical engineer Rohan Shirwaiker. “It’s a force for bringing people together with different expertise to carry these projects through.”
Targeting something as complex as biofilm-associated infections benefits from such a team approach.
Biofilm colonies live within a difficult-to-penetrate extracellular matrix, and microbial cells adhere to each other within such a surface. There are numerous places where biofilms can grow. Dental plaque is biofilm. So is the pink-orange bacteria that can be found in showers, toilets and sinks. Biofilms can grow over prosthetic joints and an array of medical implants.
“Bacteria in biofilm are cloaked from the host immune system, which makes it very difficult for traditional antimicrobials to access the bacteria,” says Schnabel. “Once bacteria are in a biofilm, functions such as cellular respiration or metabolism that antimicrobials rely on to actually work are shut down. Then there’s an infection we can’t get rid of. There are many factors that make them very, very difficult infections to treat.”

That treatment challenge is addressed through the range of expertise fueling the project. Through the CMI, undergraduate scholars and graduate students are able to interact with seasoned researchers. Several have worked with Pierce and Schnabel in their biofilm research and are cited as contributors to related recently published studies.
“Our strength at the CVM is an ability to bring research to the next translational level, from animal models to eventual human use,” says Schnabel. “I think this project really shows how the connections through the CMI work. It brought together microbiology, chemistry and orthopedic surgery and led to two NIH grants.
“And the connections through the CMI allowed that to happen.”
“Yes, definitely,” adds Pierce. “The biggest thing we get through the CMI is the ability to advance science through these partnerships. Without the other person, you wouldn’t be able to do that.”
~Jordan Bartel/NC State Veterinary Medicine


