VH Hyperthyroid Clinic Revives the Feline Spirit

When her cat, Henry, starting losing weight and seemed constantly agitated, Sally Brooks’ mind flashed back 10 years.
That was when she had brought her other cat, Blackie, to the NC State Veterinary Hospital’s hyperthyroid cat clinic. The experience had been so positive that when Brooks’ primary care vet once again offered treatments options for Henry, it was an easy decision.
“I knew what was to be done — a visit to the vet school,” said Brooks.
Now, a month after his abnormal thyroid tissue was destroyed with radioactive iodine, or I-131, via a single injection under his skin, Henry is doing well. Without I-131, Brooks would have likely had to give Henry medicine twice a day for the rest of his life.
Without I-131, many cat owners are resigned to living with a pet who becomes a shell of their former selves. Hyperthyroidism, or overproduction of the thyroid hormone, raises a cat’s metabolic rate. That leads to weight loss even when eating more food.
Cats with hyperthyroidism are prone to kidney damage, as that organ works harder and faster. The condition often leads to high blood pressure and structural changes to the heart. Overactive intestines can cause vomiting and diarrhea. Cats become angrier and can look unkempt.
But by including the option of I-131, the most effective treatment for feline hyperthyroidism, the VH clinic’s cure rate is 95 percent.
“Henry,” said Brooks, “is already back to his old self.”

Both Blackie and Henry were treated by Karyn Harrell, a clinical assistant professor of internal medicine who founded the hospital’s hyperthyroid cat clinic soon after she joined the faculty in 2006. Before coming to NC State, Harrell worked with Mark Peterson, one of the founding doctors of I-131 treatment, at the Animal Medical Center in New York City.
Harrell still runs the clinic, along with associate professor Katharine Lunn and clinical assistant professor Karen Tefft. Four internal medicine vet technicians help care for cats while they are hospitalized and assist with check-up visits.
Cat owners have long been thrilled with the treatment outcome, said Harrell.
“I had one owner who was crushed by the fact that her cat slept under the covers with her and started biting her at night when he became hyperthyroid,” said Harrell. “Two weeks after treatment, he was back to cuddling with her and she was absolutely overcome with joy to have her cat back.”
Hyperthyroidism is the most common endocrine disease in older cats, but is a relatively new condition, with the first case reported in 1979, said Tefft. A pair of neck glands, the thyroid requires iodine to produce its hormone, which regulates metabolism. Feline hyperthyroidism is usually caused by hyperplasia, or overactive tissue, or an adenoma, a benign growth, said Tefft, though there is not a consensus about what leads to those conditions. In fewer than 5 percent of cases, malignant thyroid cancer is the source of hyperthyroidism.
Clients must be referred by their primary care vets to the clinic, which treats two cats a week, every week of the year. Appointments are booked about a month in advance.

There are ways to treat feline hyperthyroidism other than I-131, though each has significant drawbacks. The medication taken two times a day for the duration of the cat’s life blocks the glands from producing the thyroid hormone. But for cats, notoriously finicky about taking pills, and for owners, who balk at the thought of having their pets take pills for years, that route can be particularly burdensome. There is an alternative ointment, but it comes with several side effects.
“Twice daily medicating really disrupts the bond between many owners and their cats,” said Tefft, who joined the NC State College of Veterinary faculty in 2016. “Radioactive iodine takes that barrier away.”
Surgery to remove the overactive glands requires general anesthesia, which can be risky for older cats with heart and kidney problems. A prescription diet includes food low in iodine levels, but, said Tefft, since the thyroid is so efficient at collecting iodine, if a cat eats anything other than the diet, it will not work.
The radioactive iodine treatment is a small injection under the skin and anesthesia is not required. After a clinical consultation, the cat is injected at the start of the following week and stays at the CVM until the radiation levels the cat emits satisfactorily fall, which is usually after about four days.
At home, activity must be restricted since the cat is still radioactive; cats cannot sleep in an owner’s bed and owners need to wear gloves while cleaning a litter box. Cats return to the hospital both one month and two months after treatment for a check of thyroid levels. Cats are then seen annually.

“What I enjoy most about the service is seeing the cats back for their one-month recheck visit,” said Tefft, whose family has had cats since she was a child. “Virtually all the cats have regained some of their lost weight and have much more luxurious coats compared to when I last saw them. So many owners relate how happy they are to see their cat’s old personality back.”
Lunn has seen the same results. She started working at the clinic immediately after coming to the CVM five years ago, but treated her first hyperthyroid cat with I-131 about 20 years ago. She was part of the team that launched I-131 therapy for cats at the University of Wisconsin, then ran the first private practice I-131 clinic in the state for about a year.
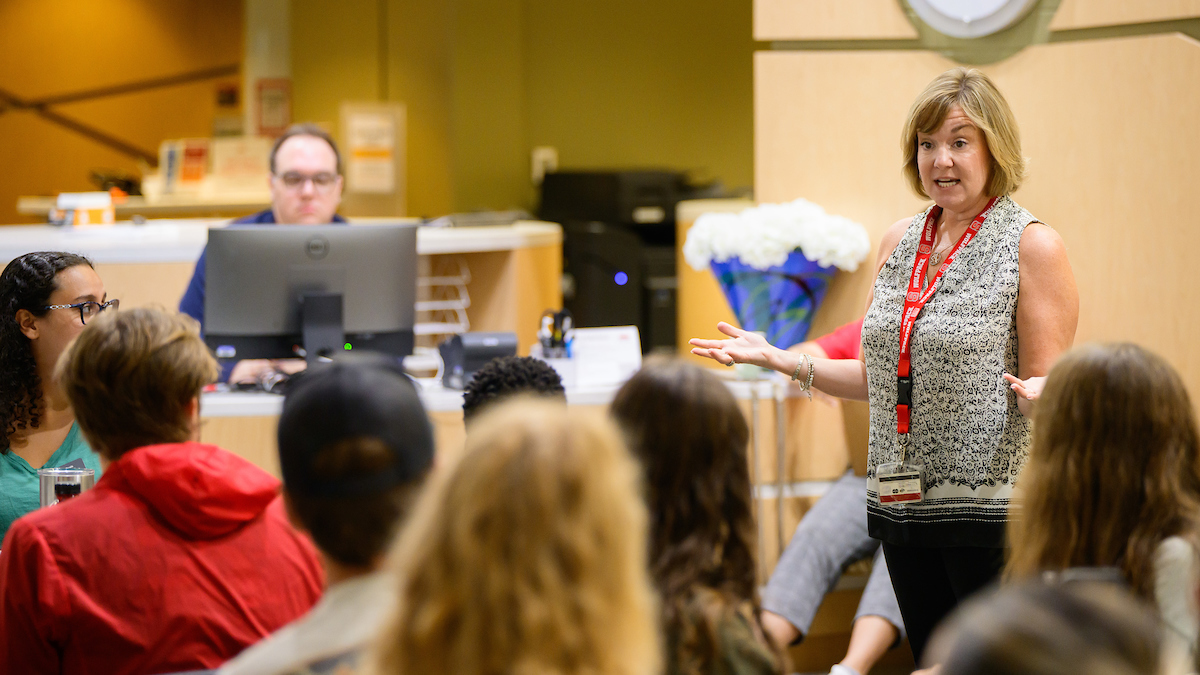
The clinic also functions as a learning center. Lunn shares many of the hyperthyroid cases with students.
“Together we can practice palpating the thyroid gland and detecting some of the other abnormalities that we find in these cats,” said Lunn. “Learning is always easier when you have real cases to relate to.”
While exploring the causes of hyperthyroidism is a big area of veterinary research, definitive answers have not been found.
Some studies have shown correlations between hyperthyroidism and fish-flavored cat food, and exposure to Bisphenol A (BPA) in food can linings and to flame retardants in carpeting. Other studies show a connection to changes in iodine levels in food. For now, Tefft recommends that owners avoid fish-flavored foods, use ceramic or metal food and water bowls and have regular vet check-ups, twice a year for senior cats more susceptible to hyperthyroidism.
For now, the hyperthyroid clinic will continue doing what it has done best over the past decade.
“The plan,” said Harrell, “is to keep going.”
For more information on the NC State Veterinary Hospital’s hyperthyroid cat clinic, click here.
~Jordan Bartel/NC State Veterinary Medicine
- Categories: