CVM Cancer Research Bridge to Human Medical Centers
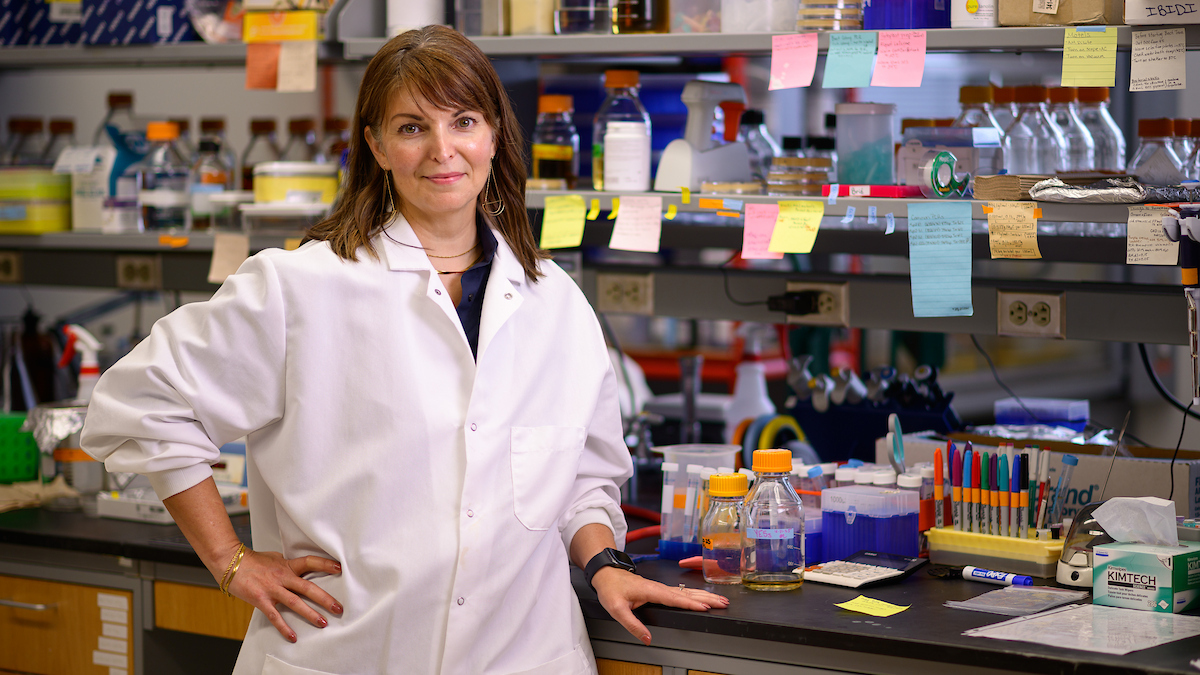
[section_subtitle]Dr. Horowitz interviewed in Technician article on NC State cancer investigations[/section_subtitle]
By Sindhu Chandramouleeswaran
During cell division, cells become damaged. These same cells multiply when they undergo the process.
The American Cancer Research Society predicts that 1,437,180 individuals will learn that they have cancer this year. To the diagnosed 10.8 million Americans, the disease is a reality they battle on a daily basis.
A single word, cancer — a group of "diseases caused by the uncontrolled growth and uncontrollable spread of abnormal cells," according to the ACRS Web site — connotes this life-changing and life-threatening disease.
Although the 5-year survival rate for patients was 50 percent in the mid-1970s, the chance for survival has increased to 66 percent, as measured by a 2003 census. Survival statistics correlate with factors such as the cancer type and stage at the time of detection. The steadily increasing survival statistics result from earlier detection and the development of new anti-cancer treatments, some of which are being developed close to home.
“There are a lot of laboratories at NCSU that are interested in cancer research, either on the basic side or the clinical side,” said Jonathan Horowitz, associate professor of oncology in the Department of Molecular Biomedical Sciences.
“If you’re in the Triangle … and somebody says ‘Who’s doing cancer research?’, probably the first thing that comes to your mind is Duke or UNC-Chapel Hill because they’re human medical centers and they are treating patients all the time," he said.
Although he said the two schools have some of the best cancer treatment centers in the country, the College of Veterinary Medicine and the College of Agriculture and Life Sciences are working on another aspect of cancer research.
"At the same time, NCSU has its own medical center, except we call it a veterinary medical center, and we see hundreds of patients every year. We have probably the best staff in the nation for veterinary oncology," Horowitz said. "Clinically speaking, there’s a lot of expertise on this campus.”
The veterinary school, he said, is a bridge to human medical centers.
"We provide novel animal models, as well as expertise and discoveries that are best tested here before moving these discoveries to a human medical center,” Horowitz said, adding that NCSU received a grant from the National Institutes of Health to "do just that." The same grant was awarded to UNC-Chapel Hill.
"We think there are a lot more similarities between our clinics and human clinics than dissimilarities," he said. "We are trying to take advantage of the expertise that we have in veterinary medicine and basic research to help push new cancer discoveries to the human bedside.”
In addition to laboratories within the College of Veterinary Medicine, a host of other scientists engage in research that is related to cancer therapeutics.
Andrew Wallace, assistant professor of environmental and molecular toxicology, is investigating two classes of drugs that are involved in chemotherapy.
One of those classes is glucocorticoids, a type of hormone that is included in most cancer therapies, he said. The other is Taxanes, a class of chemotherapeutic drugs. He said both are widely used in treating breast cancer, ovarian cancer and some small cell lung cancers.
"We’re interested in how these drugs are metabolized and how the drugs themselves modulate metabolism systems which lead to their own metabolism," Wallace said. "We are trying to understand the mechanisms behind this autoregulation.”
Wallace’s research also sheds light on the mechanisms of treatment-related side effects.
“Some people have severe toxic side effects to the drugs, while some people have no side effects," Wallace said. "We want to find out why this is. We are investigating the molecular mechanisms behind these [trends].”
Christian Melander’s laboratory is also involved in probing prospective cancer therapeutics at the molecular level. Melander, an assistant professor of chemistry whose core research is in organic chemistry, said he and his team apply "organic chemistry to problems we think have insufficient answers in the biomedical field."
“We research novel cancer chemotherapeutics. A lot of treatments have to be stopped because the person who’s sick contracts secondary infections," Melander said. "Typically, they contract these when they’re in the hospital. So we work on better ways for controlling bacterial infections, allowing the patient to go uninterrupted through a whole regimen of therapy — to increase their odds of survival.”
Sarah Amend, a senior in biological sciences, has pursued cancer research since the summer after her freshman year.
“I like the idea of finding answers to questions that will help human health, it’s very rewarding,” she said.
But cancer is a disease "that’s going to have many, many causes," Horowitz said.
“There’s not going to be a single magic bullet. There will not be one drug that cures all cancers," he said. "There are going to be a bunch of drugs, a handful of magic bullets that are administered together."
It is precisely this combination of and interaction between drugs that is of interest to Wallace’s toxicology lab.
“In most of the chemotherapeutic regimes, it’s not just one drug that’s administered," Wallace said. "It’s a cocktail of drugs. And how that cocktail not only kills cancer cells but how it affects the human metabolism pathways is of interest to my laboratory."
He is working to find the answers to questions like "how can one drug interact and cause the metabolism of another drug — and how does that affect the therapeutic level of that drug in the bloodstream?”
“So those are the two things, the yin and yang," he said. "The one side is getting enough drug to be effective and not too much drug to have severe toxicity to the patient.”
Horowitz interprets the process of discovering key information about cancer cell biology with an analogy.
“It’s a very difficult problem," he said. "Imagine working on a jigsaw puzzle that someone presents to you but they don’t give you the box. You have the pieces, but you don’t know what the picture is on the box. That’s what we do for a living. We put the pieces together without knowing what the overall picture looks like.”
Because they don’t fully know how cells operate, Horowitz said those in his laboratory "don’t know a lot of the basic details of what the wiring diagram of a cell is."
"As a consequence, if there’s a problem in the cell, often we don’t know precisely why,” he said. “Oftentimes, we may know who the culprit is, but we don’t know exactly why it’s causing trouble. Why is it that when the culprit is overexpressed or underexpressed, do cells turn into tumor cells? So, it’s a very difficult problem. The wiring diagram is complex and still a bit of mystery. And that’s why it has taken us so long to make progress in this field.”
While the secrets of cancer cell biology are yet to be fully uncovered, many commonalities have been discovered between various types of cancers.
“Lessons learned in one scenario often pay dividends in another,” Horowitz said. A laboratory focusing on one type of cancer may make research findings that are applicable to the research and/or treatment of other tumor cell types. “It’s important for people to realize that there are commonalities between tumor types as well as differences, like an overlapping Venn diagram … where some causes and therapeutic strategies will be specific for a given tumor type and other causes and therapeutics will be more general."
Horowitz also acknowledges the challenges of applying scientific discoveries to clinical medicine.
“One of the real deficits that we have at the moment is the lack of large animal models for human cancers,” he said. “There have been numerous instances where a lot of notoriety accompanied a given discovery because it worked great in mice or rats — and then it failed abysmally in humans. Why? We don’t really know. But those are the facts. These situations point out that we need new animal models beyond rodents.”
In hopes of investigating and alleviating this issue, the Center for Comparative Medicine and Translational Research was formed to find better approaches for the comparative study of various diseases of biomedical research interest.
“One of the main purposes of this center is to develop new large animal models for various human problems, including cancer," Horowitz said. "Institutions like ours are doing something to fill-in some of the gaps in the assembly line that brings a discovery from the bench to the bedside.”
Posted November 3, 2008