Chancellor’s Innovation Fund Supporting Veterinary Research
The Chancellor’s Innovation Fund at North Carolina State University is supporting the translational research of three College of Veterinary Medicine scientists working on two separate projects.
Established in 2010 by NC State with the support of Chancellor William R. (Randy) Woodson, the Chancellor’s Innovation Fund (CIF) is used for the development, protection, and advancement of ideas and discoveries and supports university scientists in developing the commercial potential of their research.
CIF support for Matthew Breen will help develop a new genetic test that will predict how long a dog diagnosed with lymphoma and treated with chemotherapy will maintain a good quality of life. The CIF is also supporting Bruce Hammerberg and Thierry Olivry in their efforts to find a new therapy that they hope will resolve chronic allergic diseases in dogs without the often unacceptable side effects of current anti-inflammatory drugs.
[section_subtitle] Supporting Canine Lymphoma Treatment Decisions [/section_subtitle]
Canine lymphoma is one of the most common cancers in dogs with an estimated 300,000 cases diagnosed annually in the United States. Without treatment, a dog with lymphoma may die within weeks. Standard chemotherapy treatment is effective for up to 85% of dogs, and 50% of these dogs will have extended quality life for at least nine months. However, opinion leaders estimate that fewer than 10,000 dogs diagnosed with lymphoma receive treatment.
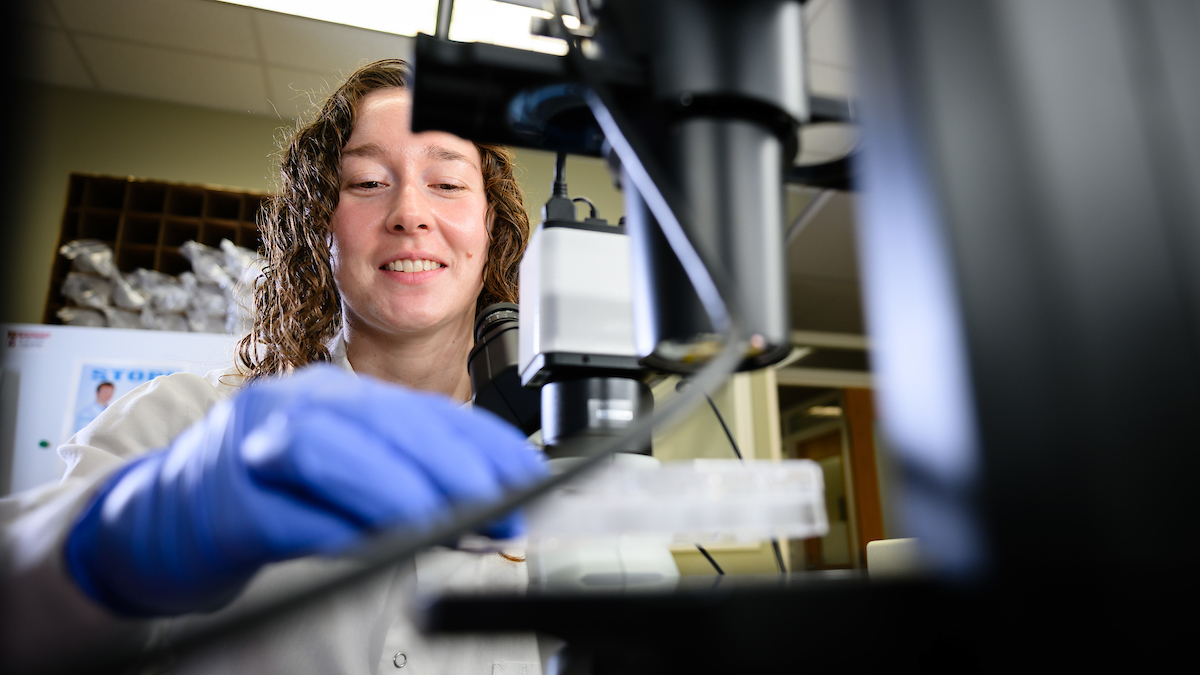
 To understand why this number is so low Dr. Breen,
To understand why this number is so low Dr. Breen,
professor of genomics
in the Department Molecular Biomedical Sciences, polled members of the 175 purebred clubs registered with the American Kennel Club. He learned major factors influencing owner treatment decisions were cost, which can range from $3,000 to $8,000 depending upon the dog, and the inability of the veterinarian to predict how long a dog on chemotherapy would live. Similar answers were given when owners of mixed breed dog were questioned.
“Many owners said they would consider treatment if they knew that their dog would have a quality of life extended to at least a year,” says Dr. Breen. “Unfortunately, there is no current prognostic test that accomplishes this. We were able to address this need as part of our boarder, ongoing program in canine cancer research. We have developed an assay that predicts the duration of first remission of canine lymphoma when treated with standard of care chemotherapy.”
The goal is for this test, which will be available to all veterinarians, is to be accurate, fast, and cost effective, according to Dr. Breen, whose laboratory is part of the Center for Comparative Medicine and Translational Research.
“Importantly, our assay makes use of the same specimen that is already obtained by a veterinarian as part of routine diagnostic work-up,” says Dr. Breen. “There will be no need to require the veterinarian to obtain and submit any new or additional samples for our assay.”
The grant from the Chancellor’s Innovation Fund will allow the research team to validate the new test on a series of patient samples and take steps to have the test be commercially available to veterinary clinics by 2014.
[section_subtitle] Treating Chronic Canine Allergic Diseases [/section_subtitle]
Dr. Hammerberg, a professor of immunology-parasitology in the Department of Population Health and Pathobiology, and Dr. Olivry, a professor of immunodermatology in the Department of Clinical Sciences, have been collaborating on allergy and clinical immunology research.
Their grant study—“Allergic Disease Therapy Using Anti-IgE Monoclonal Antibodies from Canine B Cells”—is a translation of Dr. Hammerberg’s ongoing allergic disease research and Dr. Olivry’s focus on canine atopic dermatitis. Dr. Olivry also is a senior clinician in the Dermatology Service with the Randall B. Terry, Jr. Companion Animal Veterinary Medical Center.
“Like people, dogs can suffer from various skin allergies including recurring itch and skin rashes,” says Dr. Olivry.  “When the disease can be linked to exposure to specific allergens, such as house dust mites or pollens, desensitization injections—also known as allergen-specific immunotherapy—carried out of an extended period can be effective in a few cases.
“When the disease can be linked to exposure to specific allergens, such as house dust mites or pollens, desensitization injections—also known as allergen-specific immunotherapy—carried out of an extended period can be effective in a few cases.
“Desensitization is not the answer for most dogs,” Dr. Olivry adds. “A treatment involving a combination of allergen avoidance and anti-inflammatory medication is usually prescribed. The prolonged use of these drugs, such as corticosteroids, can result in side effects, however, including increased thirst and appetite, weight gain, muscle weakness, and a predisposition to infections.”
Dr. Hammerberg says that these same challenges exist for human allergy suffers, but there has been a major breakthrough in the development of a safe and effective therapy using a humanized (engineered to be of the human sequence) mouse monoclonal antibody. This antibody specifically binds and neutralizes human IgE that is responsible for activating inflammation-producing cells responsible for allergy symptoms.
 “This product, called Xolair®, has been used safely by millions of allergy patients for more than seven years,” says Dr. Hammerberg. “Our laboratory has developed a mouse monoclonal antibody that specifically binds canine IgE in the same manner as the monoclonal antibody used to develop Xolair®. The one major obstacle remaining in providing the canine equivalent to Xolair® for treatment of allergies in dogs is generating a fully canine monoclonal antibody with the same binding properties as our prototypic anti-canine IgE mouse monoclonal antibody.”
“This product, called Xolair®, has been used safely by millions of allergy patients for more than seven years,” says Dr. Hammerberg. “Our laboratory has developed a mouse monoclonal antibody that specifically binds canine IgE in the same manner as the monoclonal antibody used to develop Xolair®. The one major obstacle remaining in providing the canine equivalent to Xolair® for treatment of allergies in dogs is generating a fully canine monoclonal antibody with the same binding properties as our prototypic anti-canine IgE mouse monoclonal antibody.”
The researchers say two approaches will be used to generate a fully canine monoclonal antibody that duplicates the therapeutic activity of the mouse monoclonal antibody. The first involves molecular engineering of the mouse monoclonal amino acid sequence to be identical to canine immunoglobulin sequence. The second approach will generate canine monoclonal antibodies from canine B cells that have the same anti-IgE epitope specificity as our mouse monoclonal antibody. Once produced, these dog-specific reagents will be tested in a proof-of concept trial to verify if they can prevent relapses of signs of allergy in some canine patients. If they do, further development will continue.