Attacking Allergies at Their Source
When it’s spring in North Carolina, you don’t need a reminder that allergies are a problem. Allergies are thought to affect about 50 million people in the U.S., impacting as many as 30 percent of adults and 40 percent of children, making allergic disease one of the leading chronic diseases in the country, according to the Asthma and Allergy Foundation of America.
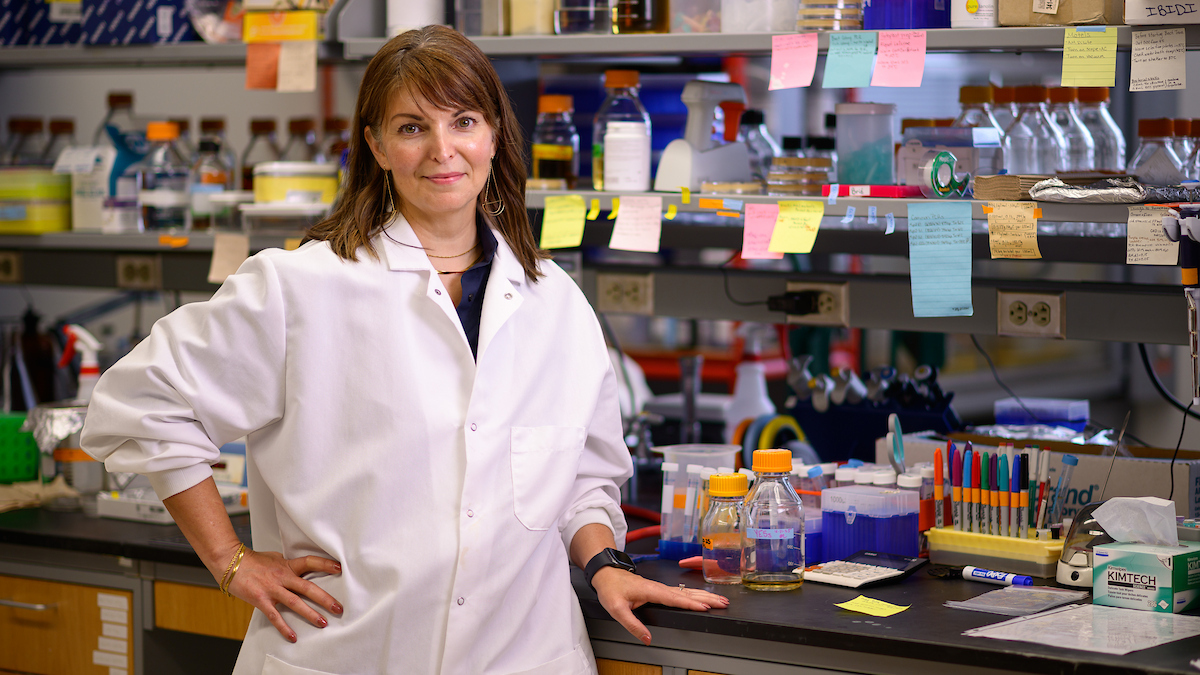
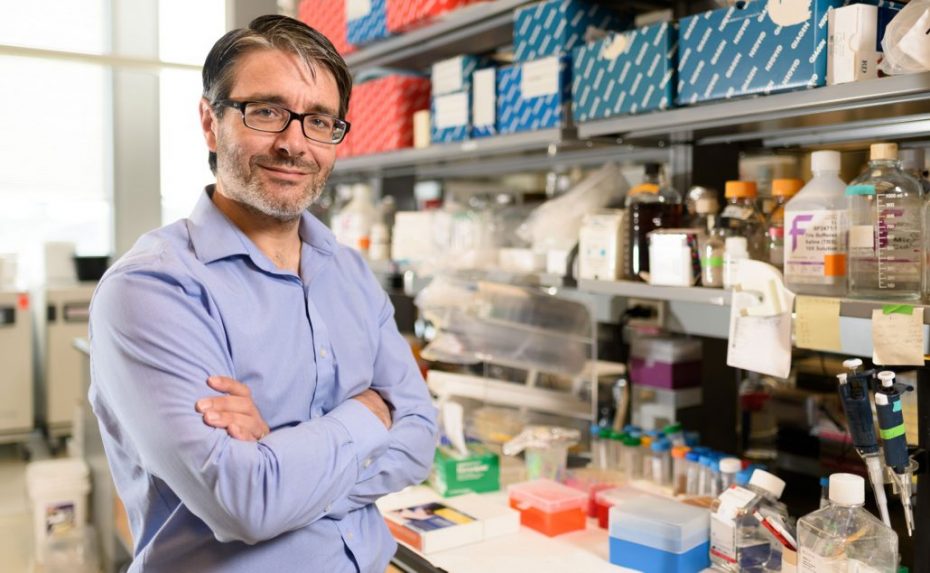
Glenn Cruse’s goal is to provide some relief. Cruse, an assistant professor of immunology at NC State’s College of Veterinary Medicine, has developed a method to stop allergic reactions by taking away a receptor from mast cells and basophils — the two main culprits, found in our tissues and bloodstreams, that drive such reactions.
Working with Dean Metcalfe, a former colleague at the National Institutes of Health, and using an RNA splicing technique called exon skipping, Cruse eliminated a portion of a gene which forms part of the immunoglobulin E (or IgE) receptor complex on mast cells that leads to certain allergic reactions. His approach attacks an allergic reaction receptor at its source, which could lead to more effective treatments for both animals and humans suffering from a range of allergies. The findings were published in the Proceedings of the National Academy of Sciences.
Cruse, a U.K. native who joined the CVM’s department of molecular biomedical sciences In January 2016, talked to us about the genesis of his work, the next frontier in mast cell research and more.
What does it mean to you to have this research published?
Finding a way in which we can target mast cells specifically has been an ongoing goal of my research for many years. Many allergic reactions come from mast cells activated by environmental allergens. There’s nothing out there that specifically targets these mast cells.
So really this has happened fairly quickly, that I’ve come up with an idea a couple of years ago and thought, “Well, this could be a way to target this gene that’s expressed explicitly in the mast cell and basophil compartments.”
From the idea to really pushing it through, it worked a lot better than I was expecting and had a really potent effect on the cells. From conception to actually having the paper out, it has been less than two years.
Take me back to that initial idea you had for the research. How did that happen?
It’s a good story. When I was studying for my Ph.D. back in England, I was looking at these genes that are mostly poorly understood. They’re expressed in immune cells, so they must be involved in an immune response. So I started to study what these genes were doing in mast cells.
I started by looking at one of these genes that was fairly well known, because this gene was part of the IgE receptor complex, and we could predict some of the outcomes making it a good starting point for developing techniques. But when I was cloning it I actually found that there was another variant that hadn’t been reported and what was meant to be a predictable starting point to study related genes ended up becoming a central part of my research. I reported the existence of this variant and then I came to the U.S., to the NIH, to study what the function of this was and eventually finding out that it functioned independently of the IgE receptor complex.
And so that then led me to really think about why it existed and why it was having a role independently of the receptor. I wanted to study more in-depth how the alteration and splicing of RNA could result in these differences in protein function and whether that had anything to do with the development of allergic disease. So I thought that by manipulating the splicing process I could study the implications of altered splicing of the gene in a physiologically relevant context without the need for gene silencing or overexpressing proteins. Once I found out that it had this really marked implication on cell function, it took a route toward translational research and therapeutic development.
What originally led to your work in allergy research?
I first became interested as an undergraduate. I didn’t know I was going to go into research in the way that I did, but at the time I knew I was interested in some kind of career in biomedical science. I ended up accepting placement in a lab doing pulmonary research and the lab was really involved in the role mast cells played in asthma.
I’ve never really looked back. I’ve been in mast cells ever since.
What kind of challenges exist in allergy research?
Allergy is a complex group of diseases, principally because the underlying causes are not clear and sometimes even the mechanisms are not clear. And you can get what appear to be allergic reactions but they’re idiopathic — we don’t know what’s causing them. That’s what keeps it interesting.
But there’s more and more things coming out. We’re showing that mast cells can be activated by any number of stimuli, such as vibration or drops in temperature. It’s a very interesting field with lots of different avenues to look at.
I know your goal is effective drug treatment. When do you hope that could be a reality?
Well, it’s in its early stages now and has a way to go yet. It’s more proof of principle for the moment, but I think that it has amazing potential. What we really need to do now is start translating it and developing the therapeutic approach. Right now I see focusing on development of ways in which we can deliver the drug into certain tissues for certain diseases and then obviously developing that with company partners, such as biotech and pharmaceutical companies to really progress it and hopefully get it into clinical trials. Obviously, being here in a vet school we can do it for a veterinary market as well. All drug development takes time, but if we can get the investment and partnerships that we need to push this forwards then things could move very quickly. Similar approaches for rare genetic diseases have proven to be very safe and well tolerated, which is encouraging.
How has the college shown their support for your research and research in general?
It’s been a very good environment. All of my colleagues have been very helpful. I see that one of my biggest challenges, and that’s with any new junior faculty, is trying to get funding. And this is one of the things my colleagues have been very helpful with.
How do you encourage students to become engaged in the type of work that you’re doing?
I think the allergy field has a lot of interest from a lot of people in veterinary medicine and just to the general population. The prevalence is really increasing at a somewhat alarming rate. And it’s showing no signs of slowing down really — not just in the human population but in the companion animal population, too. Companion animals are very prone to allergic reactions.
Whether it’s in veterinary or human medicine, it’s a field that’s not going to go away anytime soon. And it may not always be as impactful as, say, cancer research, but it’s important to people’s day-to-day lives. If you have severe eczema is can impact your mental health, too. And with asthma, I think there’s somewhere around 10 percent of patients who are not properly controlled with common therapies. There’s a real need for a more effective treatment in allergic diseases.
Tell me a little bit more about you. Where did you grow up?
I spent all of my life in England before coming to the U.S. I started in the south of England, not too far from London, in Essex. And then I moved up to the Midlands, and then for university and for my Ph.D., I went to the University of Leicester, a city which recently shot to fame because they won the English Premier League football season.
I’m assuming you are a supporter of the team.
Of course, of course. They aren’t doing so well this season, but that’s OK.
Growing up, what did you want to do?
I actually wanted to go into engineering. I was always very interested in science, but I had more of an interest in building things, so I thought about mechanical engineering. But I really didn’t know what I wanted to do and it took me a little while to figure it out. It’s not like I always thought I’d be a scientist. I never really considered it as a career when I was younger, but I always loved science.
What about science first grabbed you?
It’s just about having an inquisitive mind and wanting to know how stuff works. I wanted to just take things apart to see how they work, and then attempt to put them back together again — not always successfully.
What about research is so fulfilling for you?
It’s the finding out how things work part.
So you’re still doing that.
I’m still doing that. It’s now just taking cells apart and finding out how they work. It’s the exact same thing I used to do as a kid. And that’s why I’m interested in molecular cell biology, to work out what proteins are doing and how they’re functioning and what their role is.
What do you think of North Carolina? What has it been like for you living here so far?
It’s been much more quiet. I was in the D.C. area before. That’s busy. And it’s nice to be quiet. I do miss parts of that area. Sometimes I miss the hectic-ness and the busy-ness, but not when I’m driving. I don’t miss the traffic.
For your mast cell research, where do you hope that will be in maybe five, 10 years?
I think my research is probably an indicator of what we would like in the field, and that is to really find better ways in which we can treat mast cells specifically, depending on the disease, and the way in which the mast cells are responding. We really need a mast cell-specific drug. I’m going some way towards getting that.
~Jordan Bartel/NC State Veterinary Medicine