A Conversation with Ke Cheng, NC State University Professor of Regenerative Medicine
The ability to regenerate human tissues and organs once considered a futuristic possibility today is a fast growing medical specialty and the focus of one of the investigative cores at North Carolina State University’s Center for Comparative Medicine and Translational Research. Regenerative Medicine—the process of replacing or regenerating cells, tissues or organs to restore or establish normal function—also is one of the key components of the Chancellor’s Faculty Excellence Program, which is a strategic NC State initiative to bring “some of the best and brightest minds” to campus in a collaborative effort to solve complex issues affecting human and animal health.
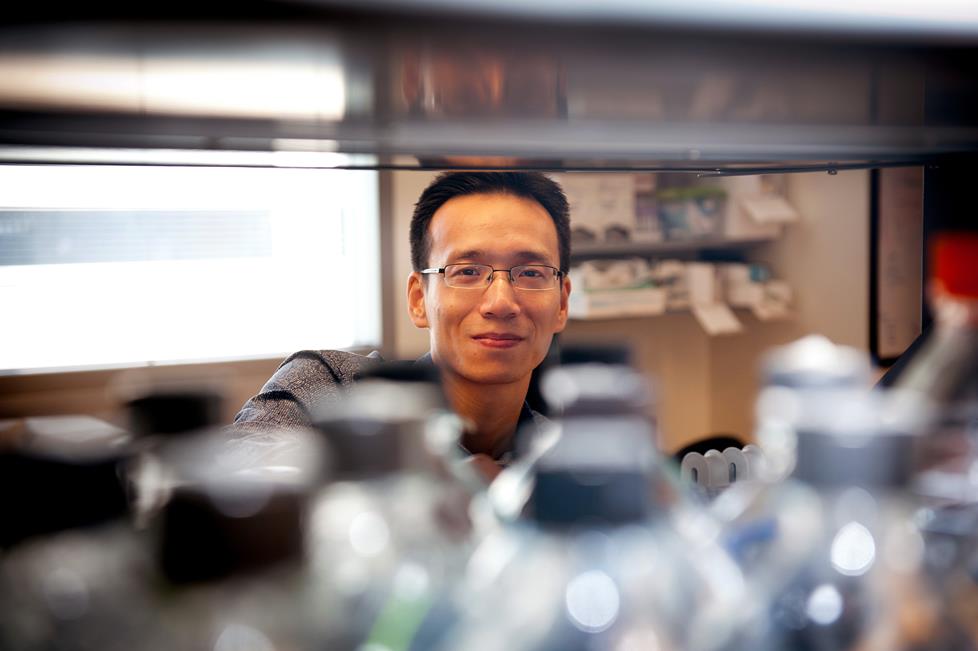
Ke Cheng, an associate professor of regenerative medicine, is one of the leading researchers recruited through the Faculty Excellence Program. Dr. Cheng’s lab is focused on translational research—taking science from the bench to the bedside. Current investigations involve using a patient’s own stem cells, biomaterials, micro-RNAs, and bioengineering approaches and testing their regenerative potential in small and large animal models of diseases.
Prior to coming to NC State, Dr. Cheng was an assistant professor at Cedars-Sinai Medical Center and University of California—Los Angeles School of Medicine, where his research focused on stem cells and regenerative medicine in animal models. Dr. Cheng also served as the director of the stem cell lab for multiple clinical trials, including the world’s first human trial using cardiac stem cells to treat heart attack.
Dr. Cheng’s research has been summarized in numerous scientific journals including Lancet, Circulation, Circulation Research, and the Journal of the American College of Cardiology, Stem Cells, Biomaterials, and Cardiovascular Research. He is an assistant editor for the Journal of Cellular and Molecular Medicine and serves on the editorial board for several other journals. Dr. Cheng’s doctoral degree is in Biological Engineering from University of Georgia.
Dr. Cheng’s appointment is part of the stated commitment to build “an internationally recognized program in regenerative medicine based on the unique opportunities available at NC State.”
[section_subtitle] Your previous research environments were Cedars-Sinai Medical Center in Los Angeles and the University of California-Los Angeles School of Medicine. What attracted you to the NC State College of Veterinary Medicine?[/section_subtitle]
I was attracted by the Chancellor’s Faculty Excellence Program cluster on translational regenerative medicine. The idea of bringing together investigators from different disciplines to advance research in both veterinary and human medicine is intriguing. This cluster initiative provides the molecular biology and engineering components needed for my work. Of course, I have the support from my home Department of Molecular Biomedical Sciences, access to the companion animal research being done at one of the nation’s top colleges of veterinary medicine, and the facilities of the Center for Comparative Medicine and Translational Research. In addition, I benefit from my joint appointment at the UNC/NCSU Joint Department of Biomedical Engineering and the resources available through that relationship. The Research Triangle Park and all of the pharmaceutical companies, universities, and research labs offer a tremendous environment for a researcher interested in both human and animal translational trials. Last but not least, I believe my previous work with human clinical studies and manufacturing human stem cells supports [CVM] Dean Paul Lunn’s vision for the CVM to reach out and be a college that is competitive in both animal and human biomedical research. This vision matches with my own research goals. All this makes NC State very attractive.
[section_subtitle] You mentioned the importance of the companion animal research being done at the CVM to your translational research studies.[/section_subtitle]
Yes. The clinical trials, the Clinical Studies Research Core, and the clinical work undertaken in Terry Center all offer invaluable data. I’m working with Bruce Keene [professor of cardiology] and Kate Meurs [professor of cardiology and Associate Dean for Research and Graduate Studies] on investigations involving animals with pre-existing disease states. If the CVM can cure that individual animal, that data may serve to help the breed and, importantly, perhaps advance human health. We will be looking at the spontaneous disease model as it appears in dogs that are brought into the Terry Center with some form of cardio distress. We want to see if we can use stem cells to treat these patients. Being able to study animals with naturally occurring diseases that relate to human disease states is critical. The mouse is a good research model for breeding and transgenic purposes and certainly is effective for bench research but if you want to understand naturally occurring diseases, you need a larger animal model. This is why Duke University Medical Center, UNC School of Medicine, Wake Forest Institute of Regenerative Medicine, and others are interested in collaborating with us. I appreciate that the CVM is focused on the One Health concept and I look forward to developing data that will allow us to take findings from our lab and translate or directly apply them to guide new therapy for humans.
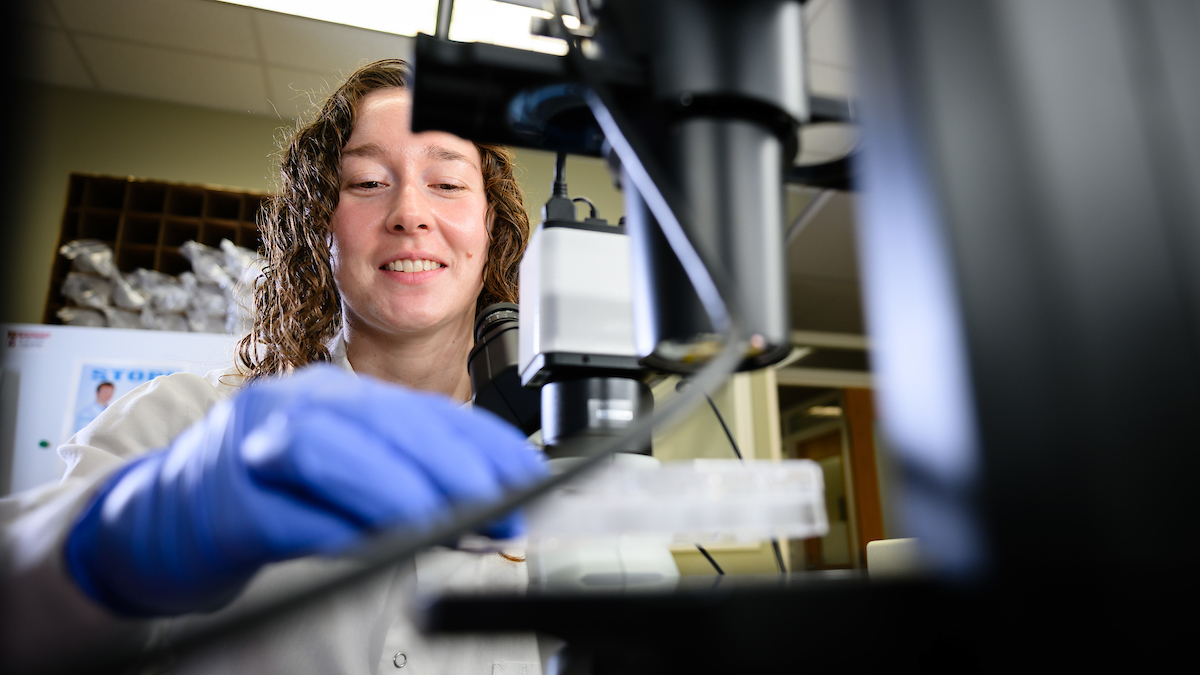
[section_subtitle] Your lab will be isolating patient-specific and organ-specific adult stem cells and testing their regenerative potential in animals. Can you briefly explain this process?[/section_subtitle]
Our focus is working with adult stem cells. Unlike embryonic stems cells, adult stem cells are partially committed and reside in a particular niche or micro-environment say, in the heart or lung or the gut. When an insult or disease happens—let’s say a heart attack—that stem cell pool expands in response to the injury. We call this an endogenous repair. The increase usually is insufficient to make the repair. You lose billions of healthy cells in a heart attack, for example, and even an expanded stem cell pool cannot compensate. Plus the environment in the post-injury heart is very hostile for these cells to survive and thrive. The concept of my research is that if these stem cells cannot expand in the organ, take them out of the organ and expand them in the lab’s supportive dish environment. We can expand the pool to an overwhelming number and then infuse these healthy stem cells back into the injured organ. These reinforcing stem cells plus the endogenous repairing mechanism have a much greater chance to offset the injury and speed the patient’s recovery from the heart attack.
[section_subtitle] What will you and your lab gain from the Joint appointment at UNC/NCSU Biomedical Engineering (BME)?[/section_subtitle]
The BME affiliation grants me an adjunct appointment at the UNC Chapel Hill School of Medicine. We will have access to human cell cultures and tissue samples that are invaluable for our lab’s regenerative studies. We also gain expertise from human medicine that will inform the design of our animal clinical trials. Since our ultimate goal is not only to cure animals but to cure people, we need to anticipate the design parameters in the potential human trial. When we submit the information for human clinical trial to the Food and Drug Administration, the FDA will examine how the trial was conducted in animals to ensure the initial design is compatible with regulations for human clinical trials. In fact, the FDA suggests researchers considering consulting with the agency for design input prior to developing an animal study. You cannot approach the FDA and say you treated mice and now want to treat humans. You need to take the trial to large animal—often time dogs, cats and pigs—before extending the trial to humans. Our partners at the UNC School of Medicine will benefit from our animal models and we will benefit from their expertise in human clinical trials.
[section_subtitle] What are your success measures and timeframe?[/section_subtitle]
I would say within five years I would like to be able to extend some data from the basic lab stage where we are now to a human test. There are many steps before that happens, of course, and I expect to work with the clinical trial people on many animal students here at the CVM. We’ll have a development team that will not only coordinate with NC State researcher but facilitate collaborations with say, UNC medical research teams, and other external scientists.
[section_subtitle] I understand you are also interested in manufacturing stem cells here? [/section_subtitle]
Yes. The vision is for NC State to become a center of stem cell manufacturing and the stem cells produced here will be sent to UNC or Duke or Harvard or Johns Hopkins or any medical institution that is participating in the trial. We are talking about this part of the plan now and having a manufacturing capability established in the next few years. This brings us back to the Chancellor’s Faculty Excellence Program. I meet biweekly in the CVM coffee shop with Binil Starly (associate professor, industrial and systems engineering) and Matt Fisher (assistant professor, biomedical engineering) who are the other two members of the translational regenerative medicine cluster. We are discussing research collaboration opportunities and preparing for this manufacturing capability. We have the manufacturing expertise in the Department of Industrial and Systems Engineering, the functional tissue engineering expertise in the Department of Biomedical Engineering, and additional expertise in the College of Textiles. All of this has the potential to create groundbreaking enterprise and center of excellence.
[section_subtitle] For more information: [/section_subtitle]
Researcher Repairs Damaged Heart Tissue with Adult Stem Cells